Hip arthrosis is a degenerative-dystrophic pathology characterized by the destruction of hyaline cartilage.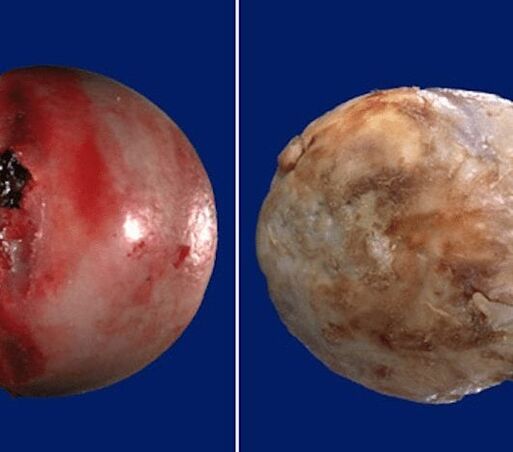 The disease develops gradually, accompanied by pain and reduced range of motion. In the initial stage of arthrosis, in the absence of medical intervention, atrophy of the thigh muscles occurs after a few years.
The disease develops gradually, accompanied by pain and reduced range of motion. In the initial stage of arthrosis, in the absence of medical intervention, atrophy of the thigh muscles occurs after a few years. The injured limb is shortened and fusion of the joint space leads to partial or complete immobilization of the hip joint. The causes of the pathology are previous injuries, curvature of the spine, systemic diseases of the musculoskeletal system.
The injured limb is shortened and fusion of the joint space leads to partial or complete immobilization of the hip joint. The causes of the pathology are previous injuries, curvature of the spine, systemic diseases of the musculoskeletal system.
Osteoarthritis is commonly seen in middle-aged patients and the elderly. Diagnosis based on the results of instrumental examinations - radiography, MRI, CT, arthroscopy. Treatment of grade 1 and 2 pathology is conservative. If ankylosis is detected or the drug therapy is ineffective, surgical surgery is performed (arthrodesis, endoprosthetics).
Mechanism of pathology development
The hip joint is made up of two bones - the ilium and the femur. The lower part of the ilium is represented by its body, which is involved in articulation with the femur, forming the upper part of the acetabulum. During movement, the glenoid fossa is motionless, the thigh head moves freely. Such a "hinged" device of the hip joint allows bending, bending, rotation, facilitates the abduction, the addition of the hip. The smooth, flexible, flexible hyaline cartilage that borders the acetabulum and the thigh head ensures unhindered sliding of the joint structures. Its main functions are to redistribute loads while moving, to prevent rapid wear of bone tissue.
External or internal factors confuse cartilage trophism. It does not have its own circulatory system - synovial fluid supplies nutrients to the tissue. In case of arthrosis it becomes thickened, it becomes viscous.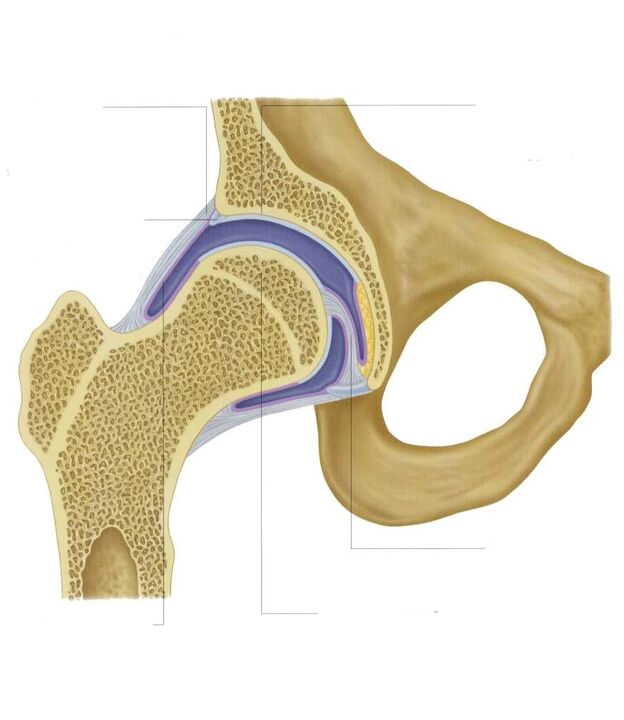 The resulting nutrient deficiency causes the surface of the hyaline cartilage to dry out. It is covered with cracks, leading to permanent microtrauma of the tissues during bending or elongation of the hip joint. The cartilage thins and loses its damping properties. The bones deform to "adapt" to the increase in pressure. Deteriorating and degenerative changes are taking place against the background of deteriorating tissue metabolism.
The resulting nutrient deficiency causes the surface of the hyaline cartilage to dry out. It is covered with cracks, leading to permanent microtrauma of the tissues during bending or elongation of the hip joint. The cartilage thins and loses its damping properties. The bones deform to "adapt" to the increase in pressure. Deteriorating and degenerative changes are taking place against the background of deteriorating tissue metabolism.
Causes and provoking factors
Idiopathic or primary arthrosis develops for no reason. Cartilage tissue destruction is thought to be due to the natural aging of the body, the slowing down of recovery processes, and the reduction in the production of collagen and other compounds needed to completely regenerate the structures of the hip joint. Secondary arthrosis occurs in the background of a pathological condition already present in the body. The most common causes of secondary disease are:
- previous injuries - damage to the ligament-tendon device, muscle cracks, their complete separation from the bone base, fractures, displacements;
- violation of joint development, congenital dysplastic disorders;
- autoimmune pathologies - rheumatoid, reactive, psoriatic arthritis, systemic lupus erythematosus;
- non-specific inflammatory diseases such as purulent arthritis;
- specific infections - gonorrhea, syphilis, brucellosis, ureaplasmosis, trichomoniasis, tuberculosis, osteomyelitis, encephalitis;
- disruption of the endocrine system;
- degenerative-dystrophic pathologies - osteochondropathy of the femoral head, osteochondritis dissecans;
- due to the hypermobility of the joints, the production of "superstretchable" collagen, which provokes excessive mobility, weakness of the ligaments.
Because arthrosis can be caused by hemarthrosis (bleeding in the cavity of the hip joint), provocative factors include hematopoietic disorders. Prerequisites for the development of the disease are overweight, excessive physical activity, and a sedentary lifestyle. Its development is caused by improper organization of sports training, lack of a diet high in micronutrients, fat and water-soluble vitamins. Postoperative arthrosis occurs a few years after surgery, especially if it has involved cutting out large amounts of tissue. The trophism of hyaline cartilage is upset by frequent hypothermia, living in an environmentally unfavorable environment, and working with toxic substances.
Hip arthrosis is not inherited. But in the presence of certain congenital features (metabolic disorders, skeletal structure), the likelihood of its development increases significantly.
Symptoms
The leading symptoms of arthrosis of the hip joint are pain when walking in the hip region, pain radiating to the groin and knee joint. One suffers from the rigidity of movements, stiffness, especially in the morning. In order to stabilize the joint, the patient begins to limp and his gait changes. Over time, the limb becomes noticeably shorter due to muscle atrophy and deformation of articulation. Another characteristic sign of pathology is the restriction of hip abduction. For example, difficulties arise when trying to sit in a chair with legs apart.

In the first severity of arthrosis, intermittent pain occurs after intense physical exertion. They localize in the articulation area and disappear after a long rest.
With second-degree arthrosis of the hip joint, the severity of the pain syndrome increases. The discomfort occurs even at rest, extending to the thighs and groin, increasing with weight lifting or increased motor activity. To eliminate the pain in the hip joint, a person begins to limp imperceptibly. Note the restriction of joint movement, especially during thigh abduction and internal rotation.
Third degree osteoarthritis is characterized by constant severe pain that does not decrease day or night. Difficulties arise when moving, so one is forced to use reeds or crutches while walking. The hip joint is stiff and the muscles of the buttocks, thighs and legs have significant atrophy. Due to the weakness of the abductive thigh muscles, the pelvic bones move in the frontal plane. To compensate for the shortening of the leg, the patient leans towards the injured limb when moving. This causes a strong shift in center of gravity and an increase in joint stress. At this stage of arthrosis, pronounced ankylosis of the joint develops.
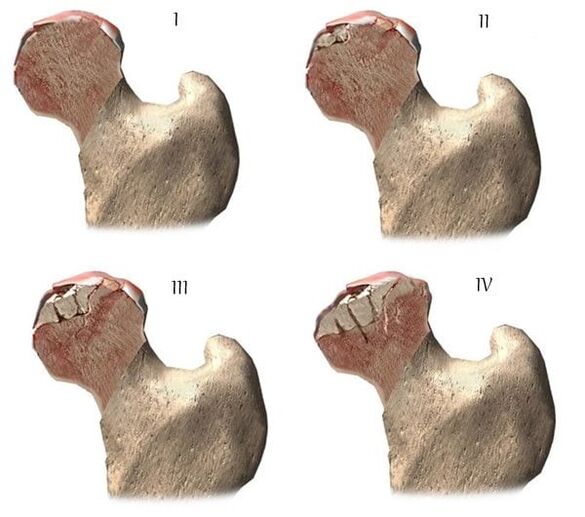
| Degree | Radiographic signs |
| The first | The changes are not pronounced. The joint gaps narrowed moderately and unevenly, with no destruction of the femur surface. Minor bone growths are observed at the outer or inner edge of the acetabulum |
| The second | The height of the joint space is significantly reduced due to uneven fusion. The bony head of the femur shifts upward, deforms, enlarges, its contours become uneven. Bone growths form on the surface of the inner and outer edges of the glenoid fossa |
| Third | There is a total or partial fusion of the common space. The thigh head was strongly dilated. There are several bone growths on each surface of the acetabulum |
Diagnostics
In making the diagnosis, the physician will take into account the clinical manifestations of the pathology, the medical history, the results of the patient's external examination, and instrumental examinations. Radiography is the most informative. It is used to assess the condition of the hip joint, the stage of its course, the degree of damage to the cartilage tissues, and in some cases to determine the cause of the development. If the cervico-diphyseal node is enlarged and the acetabulum is oblique and flattened, a dysplastic congenital change in articulation is most likely to be assumed. Perthes disease or juvenile epiphysiolysis is indicated by a disturbed shape of the hip bone. Radiography may reveal post-traumatic osteoarthritis, even though there was no previous history of trauma. Other diagnostic methods are also used:
- CT helps to recognize the growth of the edges of bone plates, formed osteophytes;
- MRI is performed to assess the condition of connective tissue structures and the extent of their involvement in the pathological process.
If necessary, the inner surface of the joint is examined with arthroscopic instruments. Differential diagnosis is performed to exclude gonarthrosis, lumbosacral, or thoracic osteochondrosis. Pain in arthrosis can be disguised as a clinical manifestation of radical syndrome caused by nerve entrapment or inflammation. Neurogenic pathology can usually be ruled out using a series of tests. Hip arthrosis is necessarily distinguishable from trochanteric bursitis of the hip joint, ankylosing spondylitis, and reactive arthritis. Biochemical studies of blood and synovial fluid are performed to rule out autoimmune pathologies.
Medication tactics
The goal of medical treatment is to improve the well-being of the patient. For this purpose, drugs belonging to different clinical and pharmacological groups are used:
- non-steroidal anti-inflammatory drugs (NSAIDs) - Nimesulide, Ketoprofen, Diclofenac, Ibuprofen, Meloxicam, Indomethacin, Ketorolac. Injectable solutions are used to relieve acute pain, tablets, pills, ointments, gels help to relieve mild to moderate pain;
- glucocorticosteroids - triamcinolone, dexamethasone, hydrocortisone. It is used in the form of intra-articular blockades in combination with Procaine, Lidocaine anesthetics;
- muscle relaxants - Baclofen, Tizanidine. They are part of a treatment regimen for skeletal muscle spasm, a tightening of sensitive nerve endings;
- drugs that improve blood circulation in the joints - nicotinic acid, aminophylline, pentoxifylline. Patients are required to improve tissue trophism, prevent disease progression;
- chondroprotectors. It is effective only in stages 1 and 2 of arthrosis.
Rubbing with warming ointments will help relieve mild pain. The active ingredients of the external agents are capsaicin, cinquefoil, camphor, menthol. These substances are characterized by local irritating, disturbing, analgesic effects. Compression of the joints with dimethyl sulfoxide, medical bile helps to cope with swellings, morning swelling of the thighs. Classical, acupressure, or vacuum massage is recommended for patients with coxarthrosis. Daily exercise is an excellent prevention of further progression of osteoarthritis.
Surgical intervention
Surgery is performed with the ineffectiveness of conservative therapy or the diagnosis of pathology complicated by ankylosis. Cartilage of the joint damaged by arthrosis cannot be restored without prosthetic surgery, but with the right approach to treatment, adherence to all medical prescriptions, maintaining a proper lifestyle, therapeutic practices, regular massages, eating vitamins and proper nutrition, you can stop cartilage and hip jointsand destruction.






















